Getting a stent saved your life. But your journey doesn’t end when you leave the hospital. What you do after angioplasty determines whether you stay healthy or face problems again.
Here’s a sobering fact: In-stent restenosis (re-blockage) occurs in about 1 in 4 patients who undergo angioplasty with stenting. The good news? Most cases are preventable with proper care.
Many patients make dangerous mistakes. They think a stent means they’re “cured.” They skip medications, ignore lifestyle changes, and miss follow-ups. Don’t be one of them. This guide explains everything you need for long-term success after your procedure.
Understanding Life After Angioplasty
Your stent opened a blocked artery. It restores blood flow to your heart. But it didn’t fix what caused the blockage in the first place.
What your stent does:
- Keeps the artery open permanently
- Prevents immediate re-narrowing
- Restores normal blood flow
- Relieves chest pain and symptoms
What your stent doesn’t do:
- Cure heart disease
- Stop plaque formation in other arteries
- Prevent future blockages
- Eliminate risk factors
Think of your stent like a bridge over a damaged road. The bridge helps you cross today. But you still need to maintain the entire road system to prevent future problems.
What “After-Care” Really Means
After-care isn’t optional. It’s essential for preventing complications and ensuring long-term success. Most people can resume routine activities within two weeks after angioplasty and stent placement, but ongoing lifestyle changes are essential for long-term heart health.
The Five Pillars of Post-Angioplasty Care
1. Medication adherence: Taking prescribed medicines exactly as directed every single day without missing doses.
2. Risk factor control: Managing blood pressure, blood sugar, and cholesterol to target levels.
3. Lifestyle modification: Adopting a heart-healthy diet, regular exercise, stress management, and quitting tobacco.
4. Regular follow-ups: Scheduled visits with your cardiologist to monitor progress and detect problems early.
5. Symptom awareness: Recognizing warning signs that require immediate medical attention.
All five pillars work together. Neglecting even one increases your risk of complications.
Essential Medications: Your Daily Protection
Medications are not optional after angioplasty. They prevent blood clots, control risk factors, and protect your heart.
Blood Thinners (Antiplatelet Drugs)
Dual antiplatelet therapy (DAPT): Most patients take two blood thinners for the first 6-12 months.
- Aspirin: Usually lifelong (75-150 mg daily)
- Second drug: Clopidogrel, ticagrelor, or prasugrel for 6-12 months
Why it matters: Blood thinners prevent clots from forming on your stent. Stopping them too early dramatically increases risk of stent thrombosis (sudden blood clot), which causes heart attacks and death.
Never stop blood thinners without consulting your cardiologist. Even if you need another surgery or dental work, talk to your doctor first about the safest approach.
Cholesterol Medications
Statins: High-intensity statins are essential after angioplasty.
- Atorvastatin 40-80 mg or Rosuvastatin 20-40 mg
- Reduces LDL cholesterol
- Stabilizes existing plaques
- Prevents new blockages
Target: LDL cholesterol below 70 mg/dL, ideally below 55 mg/dL
Blood Pressure Medications
ACE inhibitors or ARBs: Protect your heart and blood vessels even if blood pressure is normal.
Target: Blood pressure below 130/80 mmHg
Additional Medications
Beta-blockers: If you had a heart attack or have weak heart muscle
Diabetes medications: If you’re diabetic, maintaining tight sugar control is critical
Why Post-Procedure Care is Essential
In-stent restenosis typically occurs within three to six months after treatment. Proper care during this critical period is vital.
Preventing Restenosis (Re-Blockage)
Your body’s natural healing response can sometimes go wrong. Scar tissue forms inside the stent, narrowing the artery again. This is called restenosis.
Modern drug-eluting stents have dramatically reduced restenosis rates. With proper care, re-blockage occurs in less than 10% of patients with drug-eluting stents.
Protecting Other Arteries
Your stent fixed one blockage. But heart disease affects your entire circulatory system. Without lifestyle changes, new blockages develop in other arteries.
Preventing Heart Attacks and Strokes
Post-procedure care reduces your risk of future cardiac events by 50-70%. This isn’t just about your stented artery—it’s about protecting your entire cardiovascular system.
Common Mistakes Patients Make
Don’t sabotage your recovery with these dangerous errors:
Mistake 1: “I’m Cured, I Don’t Need to Change”
The truth: Your stent treated a symptom, not the disease. Without lifestyle changes, new blockages will develop. Heart disease is chronic and requires lifelong management.
Mistake 2: Stopping Medications Too Soon
The truth: Stopping blood thinners early causes stent thrombosis in up to 30% of patients. This often results in heart attack or death. Never stop medications without your cardiologist’s approval.
Mistake 3: Skipping Follow-Up Appointments
The truth: In-stent restenosis doesn’t always cause symptoms. Regular checkups detect problems before they become emergencies. Many patients discover re-blockage during routine follow-ups.
Mistake 4: Returning to Old Habits
The truth: Resuming smoking, unhealthy diet, or sedentary lifestyle undoes your stent’s benefits. These habits caused your heart disease in the first place.
Mistake 5: Ignoring New Symptoms
The truth: New chest pain, unusual fatigue, or breathlessness could signal problems. Report symptoms immediately rather than waiting.
Your Heart-Healthy Lifestyle Plan
Lifestyle changes are as important as medications. Here’s your practical action plan.
Diet: What to Eat After Angioplasty
Focus on these heart-healthy foods:
Whole grains:
- Brown rice, whole wheat roti, oats
- Replace white rice with brown or red rice
- 3-4 servings daily
Fruits and vegetables:
- 5-7 servings daily
- All colors for maximum benefits
- Fresh is best, frozen is acceptable
Lean proteins:
- Fish (2-3 times weekly, especially salmon and mackerel)
- Chicken without skin
- Legumes (dal, rajma, chole)
- Limited red meat (once monthly)
Healthy fats:
- Nuts (handful daily, unsalted)
- Olive oil or mustard oil for cooking
- Avoid vanaspati ghee and trans fats
Foods to avoid:
- Salt: Less than 5 grams (1 teaspoon) daily
- Processed and packaged foods
- Deep-fried items
- Sweets and sugary drinks
- Full-fat dairy products
Sample daily meal plan:
- Breakfast: Oats porridge with fruits and nuts OR 2 egg whites with vegetables
- Mid-morning: Fresh fruit
- Lunch: 2 rotis + dal + vegetable + salad + buttermilk
- Evening: Green tea + handful of roasted nuts
- Dinner: Light meal – vegetable soup + 1 roti OR khichdi with curd
Exercise: Moving After Your Stent
After angioplasty and stent placement, it’s key to start a safe exercise routine. Physical activity strengthens your heart and prevents future problems.
Week 1-2 after procedure:
- Gentle walking 10-15 minutes, 2-3 times daily
- Avoid lifting anything heavier than 5 kg
- No strenuous activities
- Rest when tired
Week 3-4:
- Increase to 20-30 minutes continuous walking
- Can resume most daily activities
- Still avoid heavy lifting
Week 5 onwards:
- Build to 30-40 minutes daily brisk walking
- Can add light resistance exercises
- Consider cardiac rehabilitation program
Long-term exercise plan:
- 150 minutes moderate exercise weekly (30 minutes, 5 days)
- Brisk walking is perfect
- Add yoga or stretching 2-3 times weekly
- Swimming or cycling are excellent alternatives
Warning signs to stop exercise:
- Chest pain or pressure
- Unusual shortness of breath
- Dizziness or lightheadedness
- Irregular heartbeat
- Excessive fatigue
Stress Management
Chronic stress damages your heart and increases cardiac risk.
Daily stress-reduction techniques:
- Meditation: 10-15 minutes daily
- Deep breathing: Practice when stressed
- Yoga: 20-30 minutes, 3-4 times weekly
- Adequate sleep: 7-8 hours nightly
- Social connections: Spend time with loved ones
- Hobbies: Engage in activities you enjoy
Quit Tobacco Completely
Smoking after angioplasty dramatically increases re-blockage risk. Even one cigarette daily is dangerous.
Benefits of quitting:
- Re-blockage risk drops by 50%
- Future heart attack risk decreases
- Overall cardiovascular health improves
Ask your doctor about smoking cessation programs if you need help quitting.
Follow-Up Schedule: When to See Your Cardiologist
Regular follow-ups detect problems early when they’re easiest to treat.
Standard Follow-Up Timeline
First month:
- Visit 1-2 weeks after discharge
- Check wound healing
- Adjust medications if needed
- Discuss activity level
First 3 months:
- Monthly visits
- Monitor blood pressure, sugar, cholesterol
- ECG at each visit
- Adjust medications to reach targets
3-12 months:
- Every 3 months
- Continue monitoring
- Stress test at 6 months (if needed)
- Echocardiogram at 6-12 months
After 1 year:
- Every 6 months if stable
- Annual comprehensive checkup
- Repeat tests as recommended
Tests You May Need
Routine tests:
- Blood pressure monitoring
- Blood tests (lipid profile, blood sugar, kidney function)
- ECG
- Echocardiogram
Additional tests if symptoms develop:
- Stress test (TMT)
- CT coronary angiography
- Repeat coronary angiography (if needed)
When to Seek Immediate Help
Contact your doctor or go to emergency room if you experience:
Emergency symptoms:
- Chest pain lasting more than 5 minutes
- Chest pain different from before your stent
- Severe shortness of breath
- Fainting or severe dizziness
- Rapid or irregular heartbeat
Urgent symptoms (call doctor same day):
- New or worsening chest discomfort
- Unusual fatigue that limits activities
- Swelling in legs or ankles
- Any symptoms similar to before your stent
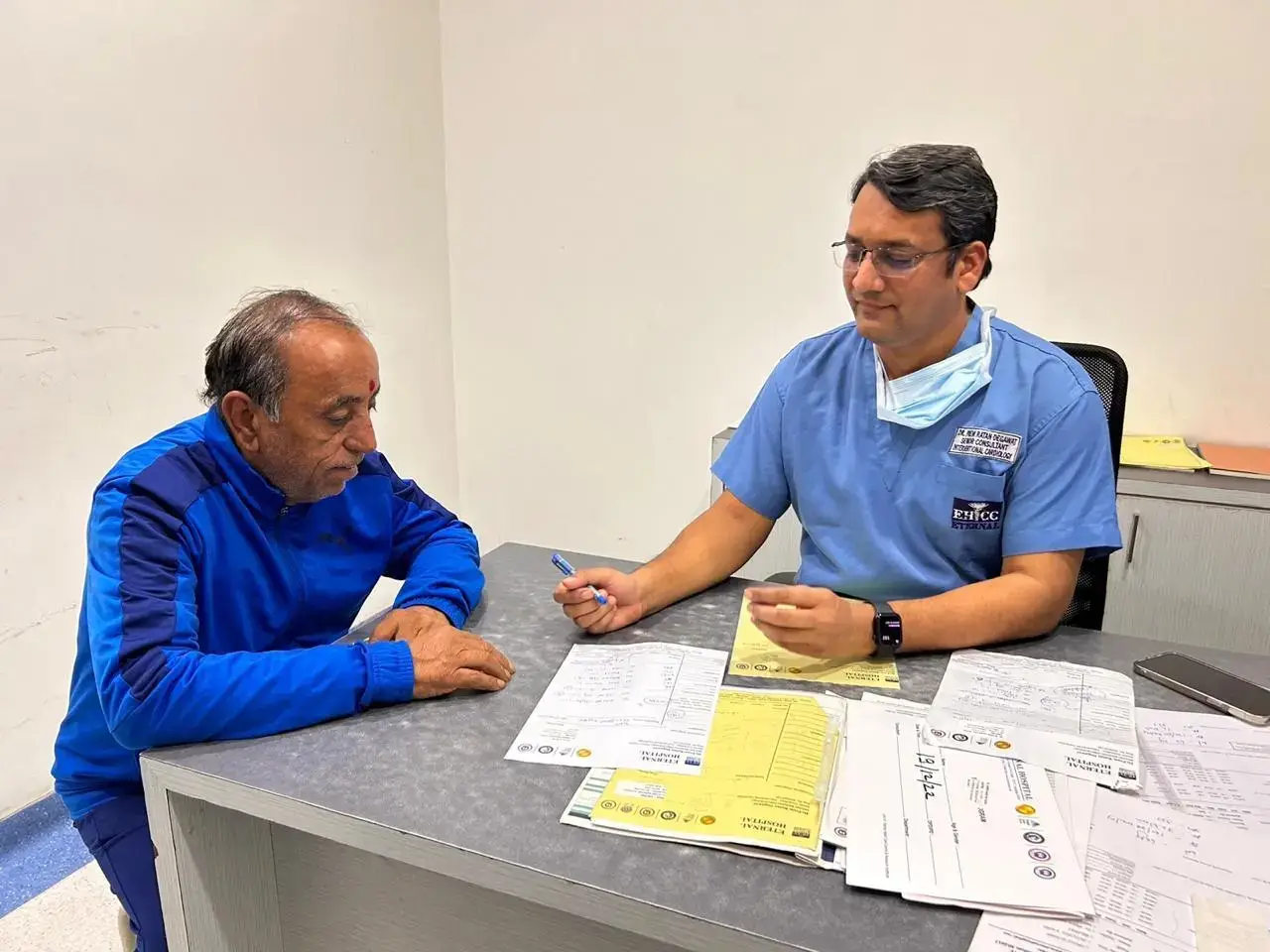
Dr. Prem Ratan Degawat: Your Long-Term Care Partner
Post-angioplasty care requires expertise and ongoing support. Dr. Prem Ratan Degawat provides comprehensive follow-up care in Jaipur.
Specialized Post-Procedure Care
What Dr. Degawat offers:
- Personalized medication management
- Regular monitoring and adjustments
- Advanced diagnostic testing when needed
- Lifestyle counseling and support
- Cardiac rehabilitation guidance
- 24/7 emergency access for concerns
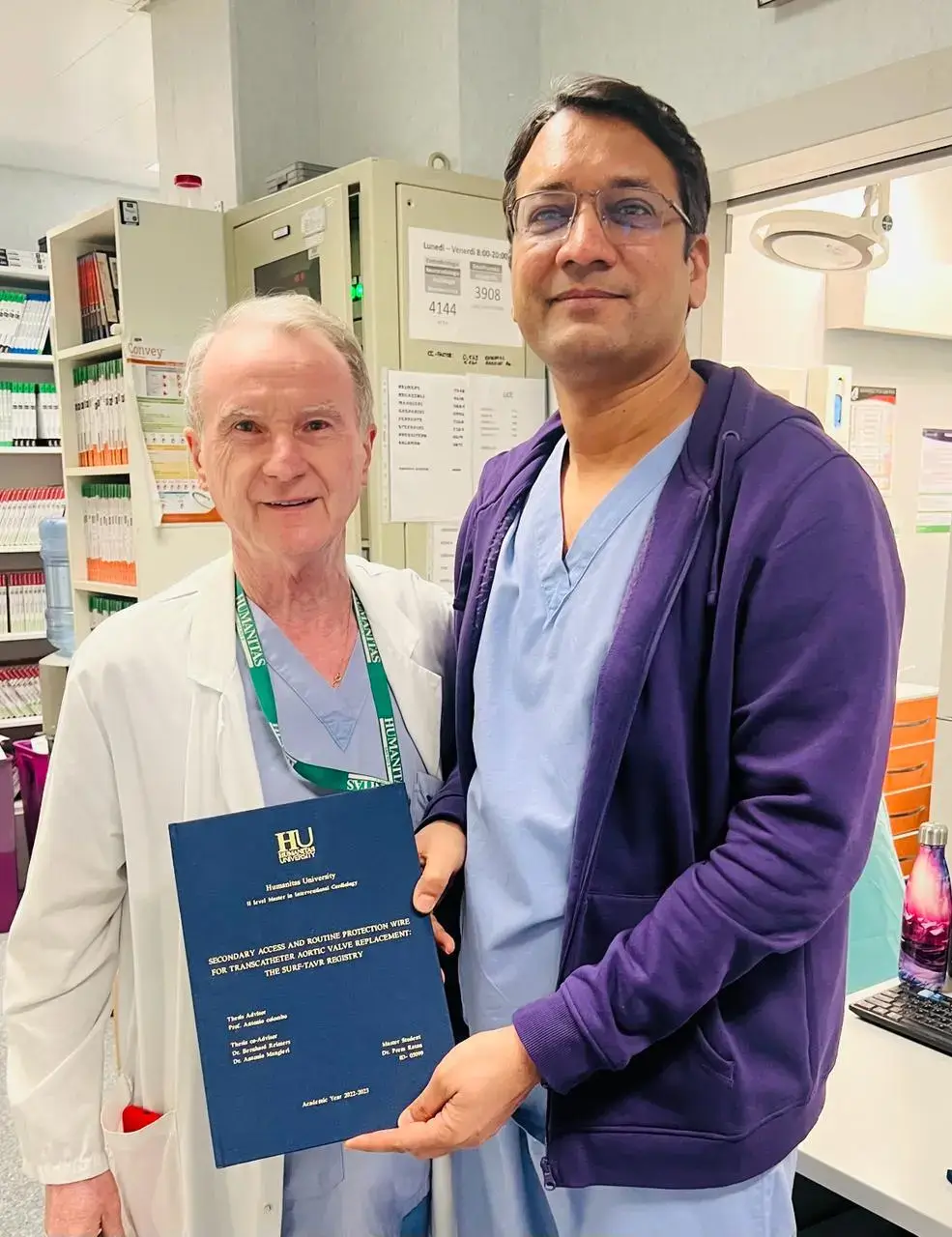
Experience and expertise:
- 15+ years in interventional cardiology
- Thousands of successful procedures
- 99% success rate
- Expert in managing complex cases
Comprehensive care:
- Focus on prevention and long-term health
- Evidence-based treatment protocols
- Patient education and empowerment
- Accessible, affordable care in Jaipur
Patient-centered approach:
- Thorough explanations of your condition
- Shared decision-making
- Ongoing support and guidance
- Transparent communication
Your Action Plan: Starting Today
This week:
- Take all medications exactly as prescribed
- Start or continue daily walking
- Make one dietary improvement
- Schedule your follow-up appointments
This month:
- Reach target exercise level (30 minutes daily)
- Implement heart-healthy meal plan
- Achieve blood pressure and sugar targets
- Complete all recommended tests
Ongoing:
- Never miss medications
- Maintain healthy lifestyle consistently
- Attend all follow-up appointments
- Report new symptoms promptly
The Bottom Line
Your stent gave you a second chance. What you do with this chance is up to you. Patients who follow post-procedure care guidelines have excellent long-term outcomes. Those who don’t often face complications.
Remember these key points:
- Your stent treated a symptom, not the disease
- Medications are essential, not optional
- Lifestyle changes prevent future problems
- Regular follow-ups detect issues early
- With proper care, most patients live long, healthy lives
Your heart health is in your hands. Take it seriously. Follow your care plan. Stay connected with your cardiologist. Make healthy choices every day.
Schedule your follow-up with Dr. Prem Ratan Degawat today. Expert care ensures your stent success continues for years to come. Your second chance at heart health deserves the best support.
Frequently Asked Questions (FAQs)
1. How long do I need to take blood thinners after angioplasty?
Aspirin is typically lifelong. The second blood thinner (clopidogrel, ticagrelor, or prasugrel) is usually needed for 6-12 months with drug-eluting stents. Never stop without consulting your cardiologist, as early discontinuation dramatically increases heart attack risk.
2. Can I exercise after getting a stent?
Yes, exercise is essential. Start with gentle walking 10-15 minutes daily in the first 1-2 weeks. Gradually increase to 30-40 minutes daily by week 5. Avoid heavy lifting for 4 weeks. Exercise strengthens your heart and prevents future blockages.
3. Will my stent block again (restenosis)?
Modern drug-eluting stents have re-blockage rates below 10% with proper care. Restenosis typically occurs within 3-6 months if it happens. Taking medications consistently, following lifestyle changes, and attending follow-ups minimizes this risk significantly.
4. What foods should I avoid after angioplasty?
Avoid salt (limit to 5g daily), fried foods, processed meats, full-fat dairy, sweets, and trans fats. Focus on whole grains, fruits, vegetables, fish, nuts, and lean proteins. The Mediterranean diet pattern is ideal for heart health.
5. When can I return to work after angioplasty?
Most patients return to desk jobs within 1-2 weeks. Physical labor may require 4-6 weeks. Your return depends on your job type, how well you’re recovering, and your cardiologist’s recommendations. Listen to your body and don’t rush.
6. Are there side effects from blood thinners?
Possible side effects include increased bleeding risk (nosebleeds, easy bruising), stomach upset, or headache. Report excessive bleeding, black stools, or blood in urine immediately. Benefits usually far outweigh risks. Never stop due to side effects without consulting your doctor.
7. How often do I need follow-up appointments?
First year: Monthly for 3 months, then every 3 months. After 1 year: Every 6 months if stable. Annual comprehensive checkup always. More frequent visits if you have symptoms or poorly controlled risk factors. Regular monitoring prevents complications.
8. Why choose Dr. Degawat for post-angioplasty care in Jaipur?
Dr. Degawat offers 15+ years of expertise, comprehensive follow-up protocols, personalized medication management, advanced diagnostic facilities, 24/7 emergency support, and patient education. He provides metro-city quality care at Jaipur’s accessible costs with proven outcomes and patient-centered approach.